

Published on Mar 14, 2024
Staff at Ambercare, a New Mexico subsidiary of Addus HomeCare (ADUS), failed to provide any services for almost 1,000 Medicaid recipients in the state, according to an internal email reviewed by The Capitol Forum and interviews with former employees of the company.
In the August 2023 email, which was sent by Melissa Benavidez, the agency director for Northern New Mexico, to staff across the state, Benavidez lists 992 clients across the company’s 22 state offices that “have not had a visit prior to 8/01/23.”
“We need to dig in and determine the reason these clients are not receiving services,” Benavidez wrote.
According to a former employee of Ambercare who worked for the company at the time, those 992 clients were all enrolled to receive personal care services, which include assistance with bathing, cooking, cleaning and other basic living activities. However, despite some clients having been enrolled with the company for several months, none of them had been visited by a home aide, who generally are supposed to come a few times per week.
Former employees of Ambercare told The Capitol Forum that a good amount, but less than half, of those clients were likely what is known as “directed care” clients, meaning that they were being cared for by a family member or friend that they had assigned as their caregiver, who would receive payments from Ambercare. The rest of the clients would receive care directly from Ambercare staff, in what is known as “delegated care.”
However, no matter who the client receives care from, Ambercare is responsible for ensuring that the clients are seen, and the vast majority of these clients were receiving their care through the New Mexico Medicaid program.
“[Managed Care Organizations] were paying about $250 per week just to have clients on our case load that we were not seeing,” the former employee said. “I recommended that we just close them out so we could release the patients to go to another company, but Ambercare wanted to hold onto them. We wouldn’t have hit our revenue targets if we had released them.”
The email shared with The Capitol Forum detailed the number of personal care clients at each of the company’s offices in the state who had not received care yet. The Capitol Forum has recreated the chart below to protect the identity of the source:
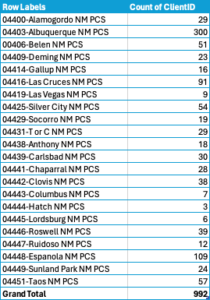
Source: Internal Ambercare Email
According to the former employee who forwarded the email, the chart indicates some massive problems at some of Ambercare’s smaller offices.
“Espanola is a small town,” the former employee said. “How could there be over 100 patients there who haven’t been seen yet? That is just a huge number for such a small place.”
Another former employee who had not seen the email but was familiar with the personal care side of Ambercare said that the numbers aligned with what they had seen during their time at the company.
Other former employees of Ambercare who were not privy to the actual data on missing personal care appointments told The Capitol Forum that it was nevertheless a massive and known problem across the company.
Because personal care clients receive help with activities of daily living, going without this assistance could have devastating effects on clients. According to a former employee, “not being seen by us means that people sometimes don’t eat or they don’t bathe. We had an obese woman who hadn’t taken a bath in two weeks.”
The revelation that hundreds of clients were going without care adds to the mounting problems at Ambercare that The Capitol Forum has uncovered, which include falsified CPR and first aid trainings for aides and failures to file critical incident reports with the state.
The New Mexico Department of Justice began a review of the company’s falsification of training documents after The Capitol Forum first reported the issue.
A spokesperson for the New Mexico Human Services Department (HSD), which oversees the Medicaid program, told The Capitol Forum that “the HSD Office of Inspector General can neither confirm or deny the existence of an investigation” but that it “takes these concerns very seriously.”
The Capitol Forum had not asked HSD if there was an investigation into the company by the department’s OIG when the spokesperson provided the above comment.
“Personal Care Services are authorized by the Managed Care Organization and the provider gets paid based on services rendered. This is verified by Electronic Verification. Managed Care Organizations audit all agency-based community benefit providers routinely. As needed, MCOs provide technical assistance to providers to ensure quality and access to care. The MCOs and HSD’s Medicaid agency are responsible for the monitoring and oversight of the provision of services delivered by registered providers,” the spokesperson said.
“It’s important for the department to ensure that everyone works together to detect, prevent, and investigate fraud, waste, and abuse in the public assistance programs administered by the Human Services Department,” the spokesperson continued, “To report public assistance fraud, waste, or abuse, including Medicaid provider fraud, we encourage the public to please visit: https://www.hsd.state.nm.us/lookingforassistance/report_fraud/”
Addus did not respond to a request for comment for this article.