

Published on Dec 21, 2022
Update: On June 6, 2024, Judge Steven Merryday entered an order dismissing Liberty Mutual’s case against EMSI with prejudice for failure to prosecute and ordered Liberty to pay EMSI’s legal fees of almost $70,000.
A Capitol Forum investigation has uncovered extensive issues regarding the billing practices of the medical device company Zynex (ZYXI), with these issues ranging from the use of improper billing codes to shipping large quantities of unnecessary supplies to patients. The NexWaves bear striking similarities to the practices of its competitor Electrostim Medical Services (EMSI).
Both Zynex and EMSI manufacture electrotherapy devices for pain management and physical rehabilitation. These devices, the Zynex NexWave and the EMSI Flex-IT, can perform both Transcutaneous Electrical Nerve Stimulation (TENS) and Neuromuscular Electrical Stimulation (NMES) using 9-volt batteries and electrodes that adhere to the skin to stimulate the muscles of patients. The NexWave and Flex-IT are also classified under the same FDA product code.
While these devices are relatively simple, 28 Liberty Mutual insurers recently sued EMSI for using billing codes associated with more complex, and expensive, devices. The insurers have also alleged that EMSI has been separating out associated resupply products and billing them separately to increase reimbursement, a practice known as unbundling.
Importantly, the complaint notes that before the company was sued by Liberty Mutual insurance companies, EMSI was sued for substantially identical billing schemes by Allstate and Nationwide. In that case, EMSI has moved to dismiss certain claims, arguing, in part, that unless state law incorporates CMS guidelines in some way, those guidelines do not apply to sovereign state laws.
Former employees of Zynex told The Capitol Forum that the company has largely stopped billing commercial insurance, mainly because those insurers stopped covering its devices. However, the former employees said that those negative commercial insurance determinations spurred Zynex to focus on billing worker’s compensation funds using questionable practices instead.
Claims data obtained from the California, New York, and Ohio state workers compensation boards through Capitol Forum public records requests show that Zynex is indeed using very similar billing practices as EMSI. Those practices could run afoul of worker’s compensation fraud and false claims act laws in those states.
Moreover, complaints made to the FTC by both Zynex customers and employees and obtained by The Capitol Forum through an additional public records request indicate that the company is deceiving patients and shipping far more supplies than necessary.
“Normal electrode usage for TENS is approximately 2-4 pairs per month, the number covered by Medicare and most commercial insurers such as Aetna,” a complaint to the FTC reads, “I have personally received over 640 pairs of electrodes from Zynex for a single prescription. Based on Medicare’s average coverage of 3-pairs per month, Zynex sent me over 20x the usual amount, enough for 18 years of constant use.”
Asked about the similarities between Zynex’s practices and the allegations raised in the EMSI complaint, a spokesperson for Zynex told The Capitol Forum that “Zynex is not aware nor involved in the allegations raised against EMSI” and said that the billing practices of the company are appropriate. Click here for the company’s full comment.
Zynex uses inappropriate billing code, according to billing data and former employee. According to the complaint against EMSI, companies selling TENS units should use the billing code E0730. If the device is intended to also provide NMES, companies can also use the billing code E0745.
EMSI, however, rarely used either of those codes to bill insurers, according to the complaint, and instead used a miscellaneous billing code for durable medical equipment, known as E1399.
“During the relevant time, the allowable reimbursement rate for a TENS/NMES unit billed under HCPCS E0730/E0745 (as appropriate) was significantly lower than the amount that could be received for E1399,” the complaint reads, “Defendants intentionally, knowingly, and fraudulently utilized HCPCS E1399 to bypass the applicable fee schedule to obtain a much higher reimbursement than allowed under the proper, applicable codes.”
A review of claims submitted to the California State Compensation Insurance Fund, the Ohio Bureau of Worker’s Compensation, and the New York Worker’s Compensation Board finds that Zynex is also using E1399 to bill for its TENS/NMES devices.
In California in 2022, Zynex used E1399 more than twice as many times to bill for its devices as the other two billing codes combined. In New York, Zynex billed the state using E1399 for about 40% of its device claims.
In Ohio, that proportion was considerably less; just 10% of device claims were submitted using E1399 in 2022.
While it is unclear why Zynex used E1399 differently in different states, any use of the billing code, according to the complaint against EMSI, is fraudulent, given that none of the companies’ devices qualify for the code. A review of the Durable Medical Equipment Coding System confirms that none of Zynex’s products are listed under E1399.
However, the Zynex spokesperson disputed this, saying that “E1399 is an accurate procedure code to be used with our NexWave device. The NexWave device is not a TENS unit, it is a multi-modality device that includes TENS, NMES, and IFC modalities. E0730 is a procedure code for TENS modality only and E0745 is for NMES only. These codes don’t accurately reflect the full spectrum of NexWave device treatment features.”
Former employees of Zynex, however, told The Capitol Forum that they knew the use of the E1399 miscellaneous billing code was inappropriate for the NexWave device when billing insurers.
“We were pressured to increase reimbursement any way we could,” a former employee in the billing department said, adding that “we were encouraged to find loopholes to meet billing goals and to avoid mandatory overtime.”
The insurers in the EMSI case also reject any nuance regarding the use of E1399, saying that “regardless of the unit, E1399 was never the correct code that should have been used – or charged – by the Defendants” because that code pertains “to oxygen equipment and supplies and is not appropriate for reporting other forms of DME especially when the DME item being supplied has a specific code.”
The insurers also argued that multimodality devices “are also classified by the FDA as TENs units. As such, these devices would be appropriately billed using HCPCS E0730.”
Monthly supplies unbundled into multiple codes. In addition to using the incorrect code to bill for its NexWave devices, Zynex also appears to be unbundling billing codes for shipments of replacement electrodes and batteries. This issue was also raised by the insurers’ complaint against EMSI.
According to the complaint, resupply of 9-volt batteries, electrodes, and lead wires should be billed together using the billing code A4595.
CMS guidance says that “billing for resupply items associated with a TENS or NMES unit is appropriate only under HCPCS A4595 regardless of the number or type of items provided,” the complaint states.
Despite this, the insurers allege that EMSI used the codes A4630, A4556, and A4557 to bill for replacement 9-volt batteries, electrodes, and lead wires separately. Moreover, the insurers note that codes A4556 and A4557 are for electrodes and lead wires that should be used in sleep apnea devices, not TENS/NMES devices.
“To the extent that the items were in fact supplied at all, Defendants’ separate billing of each supply using the codes detailed above, which misrepresent what was provided, rather than reporting HCPCS Code A4595, demonstrates Defendants’ knowing attempts to obtain significant additional unentitled reimbursements,” the complaint concludes.
The allegations made in the most recent lawsuit are backed up by expert testimony in a previous lawsuit against EMSI by Nationwide Insurance.
In the state data received by The Capitol Forum, Zynex also unbundled its claims to California, New York, and Ohio and used inappropriate codes for monthly resupplies.
For 2022, in California and New York Zynex billed A4630, A4556, and A4557 collectively far more often than they did with A4595.
In California, those three codes were billed a total of 4,926 times, whereas it billed the state using A4595 a total of 7 times. In New York, Zynex used A4595 to bill for supplies just over 1% of the time.
In Ohio, again, the company used the inaccurate codes less, but still used them to bill the state 438 times over the last year as opposed to 207 times with the correct A4595 code.
Zynex ships excessive amounts of supplies to customers, according to complaints. While Zynex may be billing state worker’s compensation boards using inappropriate codes, complaints made to the FTC and the Better Business Bureau indicate that the company is shipping far more supplies than are necessary to consumers as well.
Dozens of complaints to both organizations detail customers who were unknowingly signed up for automatic shipments of monthly supplies that pile up in their homes.
“Zynex sent me 32 packs of electrodes for the first month. Each pack contains 2 pairs of electrodes. They sent me another 32 packs the next month, and they will continue to send me 32 packs every month as long as I have the prescription. Zynex billed my insurance company $3,227 for each shipment. My insurance company paid $480 for each month,” one complaint to the FTC reads.
“Normally, patients use a maximum of 4 packs of electrodes (or 8 pairs) per month – far less than the 32 packs Zynex is sending me,” the complaint continues, “Zynex is sending me so many because my insurance company – United Healthcare (UHC) – for some reason is paying for so many electrodes. I believe Zynex is cheating UHC and its customers by taking advantage of UHC not noticing the high volume of electrodes being sent to patients every month.I believe Zynex is overcharging UHC by 10s of millions of dollars per year (I have reported this to UHC). I also believe Zynex is abusing workers compensation payors.”
On websites like eBay, patients of Zynex appear to be trying offload hundreds of unnecessary electrodes for a fraction of their cost:
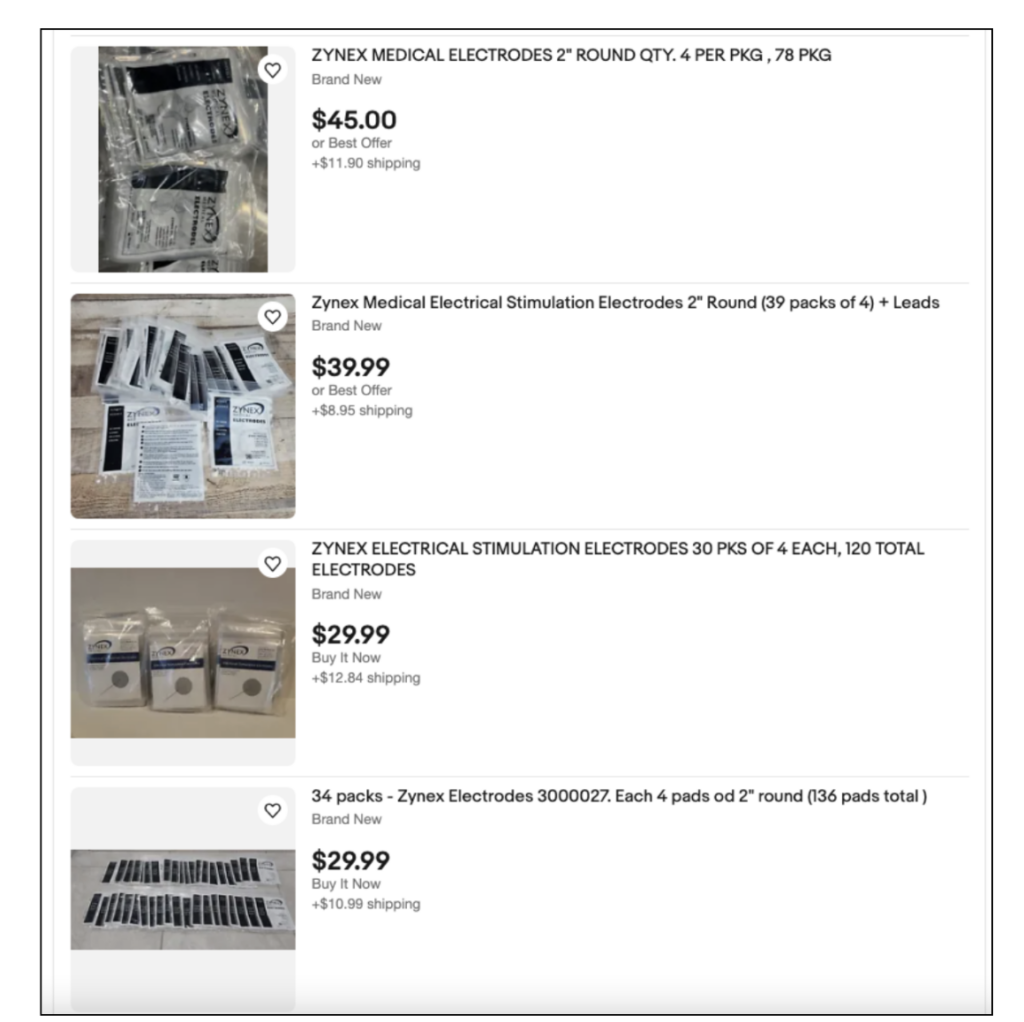
Source: ebay.com
The Zynex spokesperson disputed the notion that the company was sending too many supplies to patients, saying that “the quantity of supplies is determined based on patient’s treatment needs, as well as the quantity allowable by the patient’s insurance plan.”
“Usage can vary but many patients use the NexWave 4-6 times daily for 30-40 minutes per use,” the spokesperson continued, “To ensure effective treatment, a new pack of electrodes should be used after at least every four treatments or sooner.”
Former billing and customer service employees of Zynex, however, said that they were aware that they were sending too many supplies to customers.
“We just started seeing more and more supplies getting added to shipments,” a former billing employee said, while a former customer service employee said that “the default was to ship until the end of time, 100%. Ship as much as insurance or the patient allows, forever.”
Other complaints to the FTC indicate that some of Zynex patients appear to have done their own investigation into Zynex’s billing practices.
“Zynex collected $35 million on resales of generic 9-volt batteries and electrodes last year. Their profit margin on these items was 85%. Zynex is projected to sell $60 million this year. These products are available at retailers for approximately 10% of what Zynex is being reimbursed,” another complaint reads, “I suspect Zynex is overbilling insurers somehow (maybe by using improper coding, or unbundling the supplies code A4595 into A4630 and A4556). Insurance companies should investigate Zynex and cut reimbursement rates as the potential savings to the healthcare system and consumers is significant.”
At least one complaint also appears to have been submitted by a Zynex employee, who tipped off the FTC to false claims about the company’s products.
“I am currently an employee with Zynex Medical in Englewood, CO. I work in the warehouse for the Shipping Team,” the employee says, “A few months ago, Zynex changed the branded boxes that are shipped to all new and existing patients. The Zynex box now states Made in the USA. One of the pieces of paperwork that are sent out in each box also states Made in the USA. Zynex devices are not made in the USA at all. Zynex devices are assembled in the USA, but in no way are they made in the USA. Most if not all of the parts and pieces are imported from other countries for every Zynex device.”
“We have excellent reviews from our patients. The BBB complaints are from < 0.01% of our total patients and are typically escalations due to insurance non-coverage,” the Zynex spokesperson said.