
Published on May 11, 2023
Zynex Medical (ZYXI), a manufacturer of electrotherapy devices for pain management, is overbilling TRICARE, the military health program for active-duty soldiers and their family members, for millions of dollars in unnecessary supplies for its devices, according to a Capitol Forum investigation.
The practice mirrors those of a competitor that settled a False Claims Act matter with the Department of Justice in 2018.
As The Capitol Forum has previously reported, Zynex has a practice of sending an inordinate amount of monthly supplies, such as batteries and disposable electrodes, for its Transcutaneous Electrical Nerve Stimulations (TENS) and Nueromuscular Electrical Stimulation (NMES) devices, and billing health plans for those products.
That practice has caused the company to be kicked out of insurer networks and spurred at least two investigations by insurance companies and law enforcement, with agents specifically inquiring about Zynex’s billing practices with the federal government, according to prior Capitol Forum reporting.
While insurers have removed Zynex from their networks, The Capitol Forum received claims data from the Defense Health Agency, which oversees the TRICARE program, that show a massive spike in claims submitted by Zynex for electrodes over the last several years.
Between 2015 and 2022, the annual amount Zynex has billed TRICARE for electrodes has jumped from $1.7 million to $90.5 million, a 5,223% increase. During that period, TRICARE paid roughly 83% of those claims at a reduced fee, totaling over $42 million in payments to Zynex.
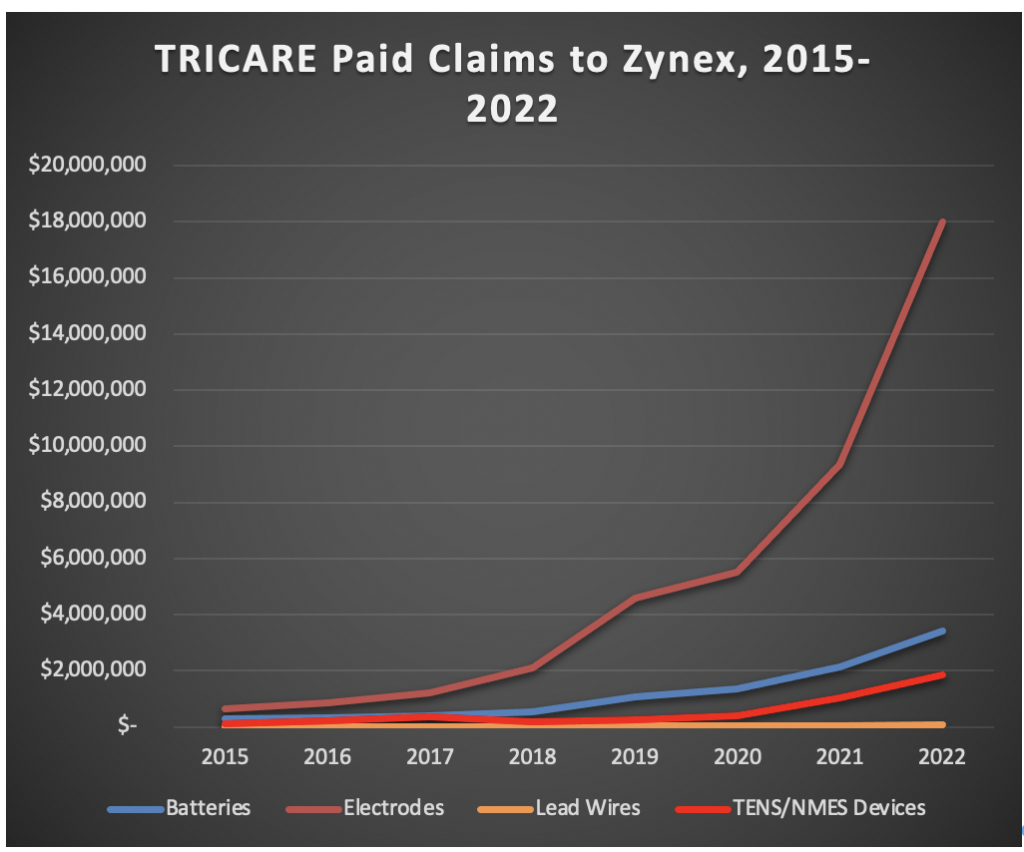
Source: Capitol Forum Analysis of DHA Data
Received Through FOIA Request
Payments for those electrodes also drastically outstrip payments for the TENS and NMES devices themselves, as well as other monthly supplies, indicating that Zynex may be sending more electrodes than necessary.
Sending unnecessary supplies to TRICARE beneficiaries could violate the False Claims Act since TRICARE is a federal health program. The DOJ, in coordination with the Department of Defense Office of Inspector General, settled a similar False Claims Act matter with the Zynex competitor Empi in 2018.
According to the press release announcing the settlement, “the settlement resolves allegations that Empi used inappropriate techniques such as ‘assumptive selling’ to persuade some TRICARE beneficiaries to seek and accept unjustifiably large quantities of TENS electrodes from 2010 through 2015, with a particularly steep increase in the number of beneficiaries receiving unnecessary quantities in 2014-2015. Assumptive selling consisted of Empi sales representatives contacting some TRICARE beneficiaries and inducing them to order excessive TENS electrodes by acting as though the beneficiaries had indicated a need for them, when that may not have been the case.”
In addition to sending and billing for too many monthly supplies, Zynex could also be liable under the False Claims Act for submitting claims using incorrect billing codes to bill for those products.
When billing TRICARE, Zynex used unbundled billing codes to bill for electrodes (A4556), batteries (A4630), and lead wires (A4557) separately. Monthly supplies for TENS units, however, should be billed using a bundled code for all three (A4595), according to CMS’ billing guidelines.
Between 2015 and 2022, Zynex received an average of $144 when billing for those products separately; had the company used the bundled supplies code, it would have received about $56 on average for each claim.
“DOJ, as well as HHS and other agencies, are working at more quickly identifying and prosecuting fraudulent billing schemes, but unfortunately it remains a challenge,” Jacob Elberg, a professor of law at Seton Hall University and a former Assistant US Attorney specializing in healthcare law, told The Capitol Forum.
“There have been numerous examples of wrongdoers identifying vulnerabilities in health care billing—especially government health care billing—where the payor will pay large amounts of money for fraudulent claims before identifying a problem,” Elberg continued, “This has been a particular issue in recent years with some compounded medicines as well as with medical devices and durable medical equipment.”
The Defense Health Agency declined to provide comment for this article. The Department of Defense and Health and Human Services OIG did not respond to requests for comment for this article.
Zynex also did not respond to a request for comment for this article.
Zynex targeted TRICARE beneficiaries as a growth opportunity. Zynex has recently targeted the TRICARE program as an area of growth for the company.
For example, an email to sales representatives sent earlier this year and reviewed by The Capitol Forum emphasized that sales representatives could earn significant commissions by focusing on TRICARE.
Company management has also noted that TRICARE claims have been a growing source of revenue for the company. During the company’s second quarter earnings call in 2020, Zynex CEO Thomas Sandgaard, asked about a recent decision by TRICARE to not reimburse TENS units for lower back pain, said that “they certainly reimburse for TENS treatment for hundreds of indications, except one indication they decided to stop covering and TRICARE is less than 5% of our business.”
“We’ve talked a little earlier about that we’ve been able to see better collections across the board on the average file. I remember having looked at TRICARE collections a few days ago and how it’s developed the last three or four months, and it’s actually increasing,” Sandgaard continued, “So we’re doing perfectly OK with TRICARE.”
While TRICARE may have accounted for 5% of the company’s business in 2020, the large uptick in electrode payments has helped push TRICARE to about 15% ($24 million) of its total revenue in 2022.
TRICARE beneficiary received thousands of dollars of unnecessary supplies; company attempted to balance bill. The Capitol Forum spoke with Sarah, a TRICARE beneficiary in New Hampshire, who received dozens of Zynex electrodes every month.
In April of 2016, a doctor prescribed a TENS device to treat a hereditary condition that caused Sarah chronic pain. Shortly after that, she began receiving huge amounts of electrodes and batteries from Zynex.
“Electrodes just started showing up at my door,” Sarah told The Capitol Forum “The doctor never said to Zynex, ‘Hey, this is how much she needs or anything’ and Zynex never called to see if I needed or wanted this many. Just every month I just got hundreds of electrodes and batteries showing up at my door. It was an obnoxious amount.”
According to Sarah’s explanation of benefits, Zynex was charging TRICARE $170 per month for electrodes and $40 per month for replacement batteries.
“No one could ever possible use this many electrodes, even if they used the device four times a day and replaced them after every single use,” Sarah said, “and the batteries last way longer than that. I have a ton of 9-volt batteries, if the world ever ends, I will be set on 9 volts.”
Sarah eventually was able to stop the shipments of electrodes and batteries in August of 2018, and since then she has been working through her existing supply which she says still takes up a bag in her bedroom and a cabinet in her kitchen.

Sarah’s Current Supply of Electrodes and Batteries
“Since 2018, I have been trying to use them up. I’ve also given electrodes to my mother and grandmother, saying, you know, ‘Hey, if you’ve got some pain, you can borrow my TENS and use up some electrodes!”
According to Sarah, several years after she was able to cancel shipments of supplies from Zynex, the company attempted to bill her for her TENS device and some supplies.
“They tried to balance bill me. Out of nowhere, in 2021, they sent me a letter demanding almost $2,000 for the machine itself. And I told them no way, you can buy one of these on Amazon for $30. Then they tried charging me for supplies for random months and amounts like one set of batteries and two sets of electrodes, in October and February, randomly. No rhyme or reason.”
TRICARE generally prohibits balance billing of beneficiaries by participating providers. Non-participating providers are limited to collecting 115% of the negotiated amount that TRICARE pays for a service or device; in 2021, the year Sarah says she received a $2,000 bill for her TENS device, TRICARE reimbursed Zynex for the purchase of one of those devices at an average rate of $127.